Don’t Be THAT Respiratory Therapist!…. (or Nurse, or PA……..)
In Respiratory school, we had to learn about the magic FI02 box. That was 32 years ago, but the strategy behind the box still works today, when thinking about Nasal cannulas, HFNC, and aerosols . Sure, today we just set a number on a machine and we’re done. Or are we?
Before you can understand anything about oxygen therapy, one must first understand Minute Ventilation.
Minute Ventilation (abbreviated Ve) is the amount of air breathed in and out in one minute. A normal, average Ve is approximately 5L in an adult. But that varies with age, size, weight, and gender. If an average Respiratory Rate is 16 and an average Vt is 5ml/Kg and an average adult weighs 70Kg, then 70 x 5 = 350 and 350 x 16 = 5600 ml or 5.6L/min.
We’ll get to what the lungs do with that 5.6 liters in a minute.
So an ‘average’ adult needs to move 5.6L of air each minute.
Hold that thought.
A patient is on a nasal cannula at 2 liters per minute.
The Nasal Cannula is attached to an oxygen green flowmeter . What percent 02 is coming out of the green tip?
The patient is on 2L of oxygen, but requires 5.6L of air every minute. Where does the other 3.6 come from?
Entrained room air, breathed in by the patient around the prongs, through the mouth, or both.
This is where it gets tricky, in so many ways….
If the flow of a device does not meet the flow requirements of the patient, it is said to be a ‘low flow’ device.
In a normally breathing, normal patient, 2 liters of oxygen translates to about 3% above 21% for each liter : 2 x 3 = 6, 21 + 6= 27% .
Now, knowing what you know about entrainment, Ve demand, and the fact that there is 100% oxygen coming out of the green tree:
Suppose this same patient is breathing at a rate of 33/min. Suppose, for example, he is in a diabetic crisis so he needs to move 8L/min to get rid of C02 to normalize his pH. What percent oxygen are we on now? Because of his high respiratory rate, and large tidal volumes, and subsequent large minute volume, he has likely diluted the FI02 down to about 22%.
Dilution and entrainment. Now let’s make matters worse:
The ABG machine made the RT guess the FI02, and on 2L the RT entered the FI02 as 27%. When you show the ABG to the MD, he or she says … Take a guess at what the MD says.
Possibly, he or she will say the FI02 is fine. Hopefully he or she will take a look at the bigger picture of Blood Gases, a topic for another day. For now, let me pose the question: how long do you think this patient can sustain breathing this hard and this fast?
As a diabetic patient, we might assume his lungs are healthy. But what if the patient is a cardiac patient? Or came in through the ED with a yet-to-be-determined diagnosis?
The moral of the story is, look at your patient. Clinical care is never based on just one piece of information.
Case study: The Oxy Mask/OxyKid/OxyTike
My last hospital used the OxyMask products. I neither endorse nor dislike OxyMask products, but you DO need to know how they work. The idea is, one mask for the full FI02 range.
Seems like a great idea… no more bins of cannulas, simple masks, non- rebreathers, just one product in 3 sizes. BUT…
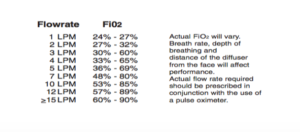
Here is a product again dependent on the patient’s respiratory rate and depth to determine a probable delivered FI02. On the attached oxygen tubing was a label, to determine the FI02. Let me interject here, the hospital had a peds floor area, but no PICU. Hence a rule was made, any kid requiring more than 40% oxygen got transferred to a nearby children’s hospital.
Here is the label:
What I want you to notice is the huge FI02 range – at 3 LPM, for example, the patient could be on anywhere from 30-60 % oxygen. The label does state that the FI02 will vary depending on the patient’s breathing pattern. But this was a nightmare for anyone not familiar with oxygen therapy. Entering the FI02 into the ABG machine was a challenge. Documenting Saturations on what FI02 was a challenge. And the higher the liter flow, the bigger the range. Only an astute healthcare person would be able to look at the patient, their respiratory rate, their work of breathing, their saturations and their color and determine what, if any changes might need to be made. We transferred lots of kids to Children’s hospital because of this.
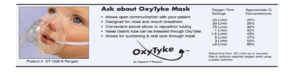
The OxyKid and OxyTyke products were at least a bit better:
Thorough assessment is the key. And understanding entrainment and dilution will help you treat your patient and adequately meet their oxygen needs.
HFNC
Knowing what you now know about low flow, high flow oxygen systems are flows that meet or exceed the patient’s minute volume demand. There are many forms of the High Flow Nasal Cannula, or HFNC. No matter what system you use, the idea is to provide enough flow to meet the patient’s demand for flow and volume, so that no room air can be entrained to dilute the FI02.
Seems easy enough until you have 2 choices of adjustments on one system: FI02 and flow. If a pediatric patient is on 4 liters per minute at 50%, what FI02 are they on? I won’t go into the full titration of HFNC here, but you do need to be aware of the fact that minute volume demand must be met. In this example, the answer is : 50% FI02. Unless the patient is outstripping the flow with his demand…. As soon as the patient needs more than 4 liters per minute, he will start entraining room air and dilute the FI02. Each system has their own method of setup and titration and weaning, and training from the company should be readily available for your staff.
21% Cool aerosol for stridor
Sometimes patients don’t need any additional oxygen, but rather a cool mist of 21% oxygen (room air). Stridor, and risk of laryngeal irritation and inflammation post – extubation often calls for cool mist to avoid any complications. All modern hospitals have both compressed oxygen and compressed air outlets. A simple trick is to put the aerosol bottle on the air flowmeter. Then, no matter where you turn the FI02 dial, it is still 21%. This is where the magic box comes in- to make sure the patient has enough flow of cool mist, so as not to entrain dry room temperature air. I have had numerous calls from pediatric nurses (and others) asking where to set the FI02 dial. When I ask, “How big is your patient?” I get a funny look. The question really is, “What is your patient’s minute volume and flow demand?” And, if they are breathing comfortably and are saturating well, we only need to meet their demands.
The equation again is: Tidal volume (for a child) = 8-10 ml/Kg. In a 20Kg kid, tidal volume might be 180-200ml. Multiplied by a comfortable respiratory rate of 30, that makes the minute volume about 6 liters per minute. But, set an aerosol at 6 L/min and not much will happen.
On the dial, it tells you what liter flow to use to obtain enough flow to maintain an FI02.
Here is the Magic Box:
100 40
60% FI02
21 40
Follow along: 100 – 60 = 40, and 60 – 20 = 40 . Meaning: If I set the venturi dial at 60%, 40/40 = 1/1, i.e. every liter of oxygen (or air) that I give will entrain 1 liter of room air.
Let’s try it with 40% :
100 20
40
21 60
Meaning: 20/60 = 1/3, thus every 1 liter of flow will entrain 3 liters of room air.
I have had RT’s go to great lengths to ensure their stridorous kid in ER has cool mist at 21% and enough flow to ensure no entrainment, only to have the nurse take it off, saying the kid was saturating at 99%. Or, the nurse thought 60% 02 (the dial setting) was too much so she turned it down to 35% (thus increasing the flow almost five-fold) .
I’ve also had nurses keep turning the flow up on desaturating kids, with no result…. Until we get a panic call.
Oxygen therapy seems so simple, but it’s easy to make a mistake if you haven’t thought through the flow and the demand, as well as the delivery device and source gas.